|
Dynamics of the doctor/patient
discussion
The structured interview is
most likely to be favourable if the dynamics follow a regulated course
(Figure).
In many cases, there is a
previous history. In a situation of expectation, the most difficult
part is at the opening of the discussion. Then follows a mutual adaptive
phase. The objective of the discussion is a definition of the
theme,
and the discussion is ended by a termination. The course of the
discussion is the result of interaction between the two partners. The doctor
is responsible for asking questions empathetically, for
listening
actively and for watching for all non-verbal signals from the
patient. His questions are aimed to obtain information which elucidates
the individual reality of the patient, and when necessary, to steer the
discussion by intervention.
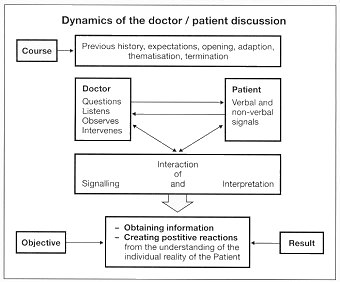 The patient acts or reacts
during the discussion, by verbal and nonverbal communications, but
can also "answer" with silence. The doctor interprets these signals
from the patient as a "participating observer". In this way he builds up
a picture of the patient, his personality, and the possible conscious and
unconscious motives in a conflict situation.
The patient acts or reacts
during the discussion, by verbal and nonverbal communications, but
can also "answer" with silence. The doctor interprets these signals
from the patient as a "participating observer". In this way he builds up
a picture of the patient, his personality, and the possible conscious and
unconscious motives in a conflict situation.
Mitscherlich termed the doctor-patient
discussion as "interaction of signals and their interpretation". From the
interpretation, the patient receives the impression: "Here is somebody
who has found out about me and does not shy away from discovering the truth
with me".
| top |
 |
|
History before the
(initial) discussion
The first doctor-patient dialogue
does not usually arise from a vacuum. Even the means by which the consultation
has come about (appointment, ward round, home visit, accident) play a decisive
role in the initial discussion. The doctor has information from the patient
himself, from relatives or from previous examinations. This means that
certain presumptions are possible before the discussion, although
these are subject to all of the dangers of prejudgment. If the patient
has a choice, the fact that he has chosen one particular doctor is significant.
The motives for a choice of doctor can be very variable; previous experience,
particular competence, reputation, age (sex) or simply because he is easily
available. Whether he was referred by another doctor, if he came of his
own accord, and if he comes alone or accompanied by relatives are also
relevant.
| top |
 |
|
Opening phase
The discussion is opened after
an expectant phase. The importance of a good opening for discussion
is dealt with in the chapter on the initiation of discussion  .
Studies have shown that the relationship between doctor and patient is
often established and structured during the first interview, and that this
markedly determines the course of further discussions. .
Studies have shown that the relationship between doctor and patient is
often established and structured during the first interview, and that this
markedly determines the course of further discussions.
| top |
 |
|
Adaptation phase/thematization
The discussion partners agree
"to accept each other" as discussion partners during the adaptation phase,
and develop a common psychical field.
Only now is it possible to
develop
a theme. Here the doctor has two important tasks; the first is to recognize
the true subject of the discussion, and secondly to steer the discussion
so that working through this subject is as effective as possible.
|
Both tasks are practically
impossible if the individual reality of the patient remains undetermined.
|
|
| top |
 |
|
Closing (termination)
The discussion should not be
broken off at random, but should be terminated according to the particular
dynamics of the course of the discussion. The length of the discussion
depends on the acuteness of the situation, the subject under discussion,
the extent to which both doctor and patient can manage, on the course of
the discussion itself, as well as on the time available. A discussion time
of more than 45 minutes will only be possible or useful in exceptional
cases.
Ideally the discussion should
be ended when the primary subject is closed, or has been taken far enough.
The discussion should be terminated if the patient shows signs of tiredness
or excessive stress, if acute resistance arises which cannot easily be
resolved, or if the discussion gets into a cul-de-sac. There should always
be a review or preliminary review. The patient should also always be given
the opportunity to put further questions. Finally, the form of further
contact between doctor and patient should be agreed.
One phenomenon which arises
at the end of a discussion should be dealt with in more detail. Often patients
are able to mention the subject that is really important to them only when
the doctor is signaling the end of the discussion. The explanation is that
the patient develops a strong defensive tendency during the conversation,
which can only be broken down when, as the end of the discussion is approaching,
he anticipates that he will not be able to discuss these points at all.
This means that questions posed at the end of a discussion or points thrown
into discussion here, can really have a very great significance.
| top |
 |
|
Technical aspects
In order that a discussion can
begin at all, it is necessary that the patient is able and ready to
speak, and the general situation is not unfavourable to the discussion.
Patients who make an appointment
and come to a surgery or practice agree to come at a certain time themselves.
On the other hand, the time of the visit of a doctor to the patient in
hospital is dictated by the requirements of the doctor. It therefore
has to be assessed if the patient is able to take part in a discussion
at a particular time, and this is not prevented by possible symptoms, pain,
hunger, thirst (being prepared for investigations), exhaustion or uncomfortable
positioning.
Problems also arise with
discussion during an examination. Occasionally, discussion can be
helped by closer physical contact during an investigation (ultrasound,
for example). It is very unfortunate when a good discussion is interrupted
by a physical examination, and the patient is left wondering whether or
not he will have an opportunity to discuss this subject again.
Opening of the interview
and further steering of the discussion should follow the so-called funnel
technique (Figure).
The method of an open introduction
with a broad unfolding is appropriate. Further questioning runs on sequential
principle. Initially the patient is allowed the largest amount of room
in which he can formulate his answers. As the discussion advances, the
contents of his answers are made more precise and clearer by decreasing
the room left for responses. This achieves a focusing of the subject
matter.
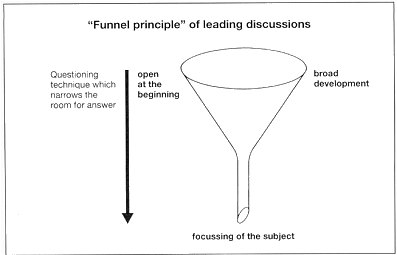 As regards the questioning
technique, the start of the discussion is accompanied by open questions
("How do you feel?", "What mood are you in?"). There are more answers that
can be given to the question: "How are you getting on?" than to the closed
question "Are things okay?" The information which is obtained is examined
more precisely by the use of an increasing proportion of closed questions.
In this way the subject is brought more and more within boundaries.
As this proceeds directive questions can be interjected, which serve
to plumb certain points ("Can you tell me more about the course of the
first attack?").
As regards the questioning
technique, the start of the discussion is accompanied by open questions
("How do you feel?", "What mood are you in?"). There are more answers that
can be given to the question: "How are you getting on?" than to the closed
question "Are things okay?" The information which is obtained is examined
more precisely by the use of an increasing proportion of closed questions.
In this way the subject is brought more and more within boundaries.
As this proceeds directive questions can be interjected, which serve
to plumb certain points ("Can you tell me more about the course of the
first attack?").
The doctor should anticipate
the patient's manner of telling his story. This depends partly on
the subject and its subjective importance for the patient, and partly on
his personality structure and character. Enough time must be available
for the discussion if details of the life history of the patient need to
be discussed.
Those who are "long-winded"
can pose a particular problem. In order to intervene, the doctor must determine
why
the patient behaves in this way. There are two main reasons. One is that
some people have a natural tendency to speak associatively. This means
that they find it difficult to stay with the point under discussion, and
what they say depends on the immediate situation or key-word which crops
up. With these people, intervention with directive and closed questions
is usually effective.
More problems are raised
in the second type of long-windedness, in which the same subject crops
up continually. Often this behaviour hides the patient's concern that he
will not be understood. Due to this, he attempts to ensure understanding
by continually repeating himself. In these cases, the following options
for intervention are available. Firstly the patient can be given strong
clear signals that his request has been understood. This can be achieved
verbally ("I am convinced that I now completely understand your problem"),
by the use of a series of questions which convince him that he has been
understood, or by using "echoing" questions ("This groin pain only happens
when you have eaten a lot of fibre?"). Another possibility is to choose
a single point as soon as convenient and go into it in detail as there
is usually less to discuss "in depth" than superficially.
A complete chapter has been
devoted to active listening  as this is the most important but also the most difficult ability for leading
discussion. The art of active listening does not only apply to what
the other is recounting, but also how he saying it and what he
does not tell.
as this is the most important but also the most difficult ability for leading
discussion. The art of active listening does not only apply to what
the other is recounting, but also how he saying it and what he
does not tell.
Meerwein points out the doctor
should also ask himself, whilst listening actively, what is happening
to him:
| • |
What
mood is the patient putting me into? |
| • |
Am I speaking
too much, too little or too impulsively? |
| • |
Am I free to
speak or inhibited by this patient? |
| • |
Do I really want
to see this patient again, or do I hope that he will never appear again? |
In other words, the doctor
must be prepared to listen not only to the patient but also to himself.
However, leading a discussion
is not limited to listening and questioning. It is necessary for the doctor
to repeatedly intervene in the conversation. One reason for intervention
can be that the course of the discussion is heading in the wrong direction,
or that it appears useless. At this point, it is helpful to introduce a
fresh, more attractive subject into the discussion in order to regain an
interactive pattern. A further reason for intervention can be to head-off
rising anxiety on the part of the patient (see chapter on anxiety  ). ).
Unwillingness to speak
may indicate defensiveness, which again requires intervention. However
the initial step is to confirm whether or not this is really defensive
behaviour. Although a break in the discussion may be interpreted as "refusal
to speak", it may in fact be a pause for decision or working through of
a point (see chapter on the pause in discussion  ). ).
If it appears from the "offer
of disease" and the preceding discussion that a conflict situation is at
the root of the physical symptoms, certain key questions serve to
elucidate the problem. Basically, a spontaneous exposure of the
conflict and working through it occurs much too infrequently in daily practice.
The grounds for this is that the patient is not really conscious of the
conflict and the doctor is not really prepared go into it. Studies from
the Heidelberg psychosomatic clinic showed that out of 100 patients referred
to the clinic, only 2 to 5 had really developed a truly conscious appreciation
of the conflicts (De Boor and Künzler). Guyotat could show that, on
the other hand, only 10 out of 75 doctors actively approached the conflicts
in their patients.
An important key question
which brings the internal conflicts into consciousness is to ask
the patient what he himself thinks are the reasons for his illness.
Von Weizsäcker formulated this question in the following way: "What
do you yourself believe to be the cause of your illness?". Meerwein recommends
the following question: "Why do you think that you are ill?". A further
aid can be to ask the patient for his own suggestions for treatment for
his illness.
It can also be important
to question, when it is clear than the patient's explanation has left "omissions
and loop-holes". Freud points out that one should "approach material at
deeper levels behind these weak points". Such holes and omissions can for
example concern certain people around the patient or his sexual life.
Nevertheless it would be
a mistake to mention conflicts too early in the discussion,
and to refer to the connection with physical symptoms. The patient does
not usually come to the doctor either aware of internal conflicts or with
the willingness to face these conflicts in discussion. When asked if they
would be prepared to speak to their doctor about personal problems, if
these had nothing to do with their illness, 73% replied "no", and only
22% "yes" (Delay and Pichot).
The basic rule of structuring
and intervention in discussion between doctor and patients has been
explained by Meerwein as follows: "None of these suggestions for intervention
in the course of discussion should deviate from the basic principle that
it is associations of the patient that define the discussion and not the
questions posed by the doctor. The questions and intervention of the doctor
arise when rationalization, omissions, contradictions, statements suggesting
anxiety and defensiveness, confrontation against the doctor and similar
forms of behaviour, influence or inhibit the development of the discussion.
The doctor needs to recognize these difficulties for what they are, and
to use them for understanding more of the illness". The final step in the
consultation interview is to establish a diagnosis and if necessary
its interpretation. The interpretation "reveals illness as being
not just a physical phenomenon but a crisis in human relationship - a conflict.
If correct and presented in a way acceptable to the patient, its result
is insight and benefit" (Meerwein). The interpretation allows worries and
uncertainties to rise to the surface, and to be put into words. This reduces
anxiety "as we rise above what we can express in words" (Nietzsche).
It can be difficult to make
a diagnosis, but even more difficult to give it an interpretation.
Meerwein lists rules which should be applied to every discussion
between doctor and patient, in which not only the diagnosis, but also the
interpretation
of the disease is required:
| • |
The
interpretation should extrapolate from what the patient himself expressed.
Therefore the patient's words, and not lofty language, should be
used. |
| • |
Interpretations
which under certain circumstances could hurt the patient should be avoided. |
| • |
The interpretation
of external conflicts should precede the interpretation of internal
conflict. Inner conflicts are rarely verbalized in conversation with doctors,
if the patient does not raise them himself. |
| • |
The interpretation is the
doctor's service, with which he compensates the patient's willingness
to converse. It encourages and reinforces the understanding
that the patient has of himself. As a result of it, the patient feels understood
and supported. This is where its therapeutic function resides. |
| top |
 |
|
The closing of the discussion
Many discussions in daily clinical
practice end as they started: unstructured and unsystematic. The end of
the conversation is far more likely to be caused by external factors (such
as situations in discussion or time-pressure) than by logical and psychological
dynamics. Nevertheless, the termination of the discussion is just as essential
a constituent as the other phases in discussion. No business discussion
about a purchase or contract would end without a clearly-defined termination.
Many discussions are "crowned" by the termination.
The end of the discussion
can be divided into 3 phases:
| 1. |
Discussion
of the conclusions |
| 2. |
Constructive
plan |
| 3. |
Parting |
Discussion of the conclusions
has more than one function: a "balance sheet" created initially.
It should make it clear to both partners what has been achieved by the
discussion. It is just as important to describe what has not been
achieved, as further discussion will depend on this, as well as the further
steps which are necessary. As at the start of the conversation, an internal
and external recognition of the other's position is once again necessary,
and should be actively sought. Summarizing at the end of the discussion
has an important control function; it reveals whether the discussion was
based on mutual reality. One objective of the summary is to round off the
discussion psychologically. Discussions which do not have recognizable
conclusions and are open-ended leave both discussion partners with a feeling
of emptiness and uncertainty. On the other hand, discussions from which
conclusions can be drawn give both parties a feeling that they have had
a quantifiable success in their discussion of a problem, that the contract
between them works, and that it is worth-while to have a discussion. The
best motivation for further discussions between doctor and patients is
a successful previous discussion.
The summary of the discussion
is a condition for the "constructive plan", which includes the following
points:
| • |
Prescriptions,
advice, suggestions, and encouragement for the patient |
| • |
Indications and
help as to how the "therapy" can be achieved |
| • |
Possibly a further
appointment |
Of course the concept of
a discussion cannot as a whole apply in every situation of daily clinical
practice (emergency situations, conversations with patients who are not
able to discuss). However wherever discussion serves as a decisive instrument
for dealing with and solving problems and conflicts, the highest degree
of efficiency is achieved with a formal, structured discussion which
is closed as regards content and subject matter.
| top |
 |
| previous page |
 |
| next page |
 |
|
|
Linus
Geisler: Doctor and patient - a partnership through dialogue
|
|
©
Pharma Verlag Frankfurt/Germany, 1991
|
|
URL
of this page: http://www.linus-geisler.de/dp/dp11_dynamics.html
|
|